April 30, 2024 ✒ Andrew Kantor
“Go to sleep or you might end up with diabetes like that man on TV.” Eat as healthily as you like, if you don’t get enough sleep you’re increasing your risk of type 2 diabetes. Using data of 250,000 people over 12 ½ years, Swedish and Chinese researchers found that people sleeping for fewer than 6 hours a night “had a notably higher risk of developing T2D compared with those with 7 to 8 hours of sleep.” And the less sleep they got, the higher the risk — even among adults with healthy eating habits. They can chow down on avocados. A study by Mexican researchers found that “Females who ate 30-38 grams of avocado had significantly lower odds of diabetes than those who did not consume avocados.” But don’t hit the guac just yet (except with a few grains of salt) — the research was out of California’s Avocado Nutrition Center. It’s now been found in a dolphin. That is all. The US had a long flu season this year, but thankfully it wasn’t a severe one and it’s just about over. That’s cold comfort to the friends and families of the 24,000 people (including 148 children) who died from the flu, but it’s a lot lower number than it could have been. Even at the peak, “we felt strained but never over-capacitated” said Dr. Jay Varkey, infectious disease physician at Atlanta’s Emory University Hospital. “It felt more like a traditional respiratory virus season than when we had massive upswings of COVID confounding it.” The birth rate in the US has been going down for decades, and after a brief pandemic “baby bump,” it’s dropped again — to the point where it’s well below the “replacement rate.” In other words, the population will begin shrinking. [T]his continued decline comes at a time of growing concern over access to reproductive healthcare and intensely politicized debate over abortion access, as well as concerns over the economy, a lack of rights for working parents and growing fears over the future of the planet. It’ll be interesting to see how debates about reproductive and immigration issues are affected. After all, if we aren’t making enough Americans, that “portends sluggish growth, an aging population and an economy that one day may struggle to find enough workers to fill jobs and pay the taxes required to maintain the state and care for a large elderly population.” The FDA has approved Utility Therapeutics’ Pivya — aka pivmecillinam — to treat uncomplicated urinary tract infections. This is the first “new” antibiotic approved for UTIs in something like 20 years. (New in quotes because Pivya is an old drug that’s been used in Canada and Europe for 40 years.) Pivya is a narrow-spectrum antibiotic […] For this reason, Pivya is only approved for use in UTIs caused by Escherichia coli, Proteus mirabilis, and Staphylococcus saprophyticus. (Links go to more details from the American Society of Health-System Pharmacists or the FDA.) A British biochemist tackles the issue: “Does ejaculating often reduce your risk of prostate cancer?” (Oh come now, we’re not going to spoil it by giving you the answer.)New/old UTI med, sleep-diabetes connection, we’re not making Americans anymore, and more!
Sleep and diabetes
If they’re women, though…
Bird flu news
But there’s good flu news, too
US birth rate keeps dropping
A “new” med for UTIs
11 new drugs in shortage
Answering the hard questions
April 27, 2024 ✒ Andrew Kantor
In case you thought the fallout from the Change Healthcare attack was ending, think again. “[T]he personal health information and personally identifiable information found in the files ‘could cover a substantial proportion of people in America’,” according to UnitedHealth. But don’t worry, it may not have included full medical histories. The company is offering two years of credit monitoring and identity theft protection to anyone who has been affected by the breach. (How to apply for that isn’t clear.) Fun fact: UnitedHealth seems to have paid the hackers a ransom of $22 million. There are good reasons to consider what time of day to take a drug — sleep issues probably top the list. But now MIT researchers have found that it’s a lot more complicated thanks to enzymes in the liver. Drug metabolism, it seems, is affected by the body’s circadian rhythm. These circadian variations affect how much of a drug is available and how effectively the body can break it down. For example, they found that enzymes that break down Tylenol and other drugs are more abundant at certain times of day. What that means is it might be possible to fine-tune the use of drugs to take advantage of this fact, setting dosing times to get the most out of a medication. We hear a lot about antibiotics to treat infections, but not so much about vaccines. That might change. Michigan State chemists have developed a carbohydrate-based vaccine (rather than a typical protein-based one) that targets Staphylococcus aureus — specifically the methicillin-resistant kind, aka MRSA. So far they’ve tested it in the lab and in animals, and obviously it works or we wouldn’t be writing about it. British researchers have just begun phase-3 trials of “the world’s first personalised mRNA cancer vaccine for melanoma,” which they are, of course, calling a “game changer.” The personalized part is what’s important, as each vaccine has to be tailored to the individual.“[A] sample of tumour is removed during the patient’s surgery, followed by DNA sequencing and the use of artificial intelligence. The result is a custom-built anti-cancer jab that is specific to the patient’s tumour.” I’m not sure what the lead investigator means by this, but it sounds good: “To be able to sit there and say to your patients that you’re offering them something that’s effectively like the Fat Duck at Bray versus McDonald’s — it’s that level of cordon bleu that’s coming to them … The patients are really excited about them.” After their work on the groundbreaking 2022 paper “Fire is Hot,” researchers at the University of Chicago have a new study — in the journal Otolaryngology-Head and Neck Surgery — with a shocking conclusion: “TikTok Riddled With Misleading Info on Health.” The team’s next paper: “What Color Is the Sky? A Multi-Modal Investigation of Lower-Atmosphere Chromatic Conditions”. People who take acid-reflux drugs — proton-pump inhibitors, H2 blockers, or even antacids — apparently have a greater risk of migraines. And if they also take magnesium, the risk is even higher. That’s what University of Maryland nutritionists discovered after parsing the health data of almost 12,000 people who used some kind of acid reducer. [T]hey found that people taking proton pump inhibitors were 70% more likely to have migraines than people not taking acid-reducing drugs. Those taking H2 blockers were 40% more likely and those taking antacid supplements were 30% more likely. They can’t prove cause and effect yet, but the relationship, they say, is definitely clear. One of the newest crop of artificial sweeteners, neotame, just went from “Well, it’s better than aspartame” to “Oh, geez, another one that’s unhealthy.” In the case of neotame, it… …can cause previously healthy gut bacteria to become diseased and invade the gut wall – potentially leading to health issues including irritable bowel syndrome and sepsis. Americans — people, insurers, and the government — spent $772.5 billion on drugs in 2023, up a whopping 13.5% from the year before. What changed? GLP-1 agonist weight loss drugs, that’s what. Spending for semaglutide doubled in 2023, making it the top-selling drug in the nation, replacing autoimmune disease drug adalimumab. Interesting side note: “Hospitals’ drug spending fell by 1.1%, continuing a steady period of falling expenditures.” Curious what the 25 most popular drugs are? Becker’s Hospital Review has you covered. The good folks at the Alliance for Pharmacy Compounding Foundation are offering $495 grants for 10 pharmacy technicians to attend a 15-hour on-demand online course, “The Ethical, Legal, and Regulatory Foundations of Pharmacy Compounding” out of Virginia Commonwealth University. If you’re interested in getting into compounding pharmacy, this is a great idea — it gives 15 hours of CE credit, not to mention a great line on your résumé. The deadline to apply is June 30, 2024 at 11:59pm EST. Here’s the link to do just that. (Got questions, contact the Pharmacy Compounding Foundation at foundation@a4pc.org. Why drug-timing matters, acid reducers bring migraines, latest TikTok shocker, and more
Chances are your data was exposed
The liver means timing matters
Two unexpected vaccines
First: against antibiotic resistance
Second: against melanoma
Science at work

From stomachache to headache
Sour sweetener
Drug spending jumps
Pharmacy techs: You could win a 15-hour course
April 25, 2024 ✒ Andrew Kantor
We’re taking some steps backward when it comes to antibiotic use. Based on the latest data*, more than a quarter of all antibiotic prescriptions are inappropriate: “[T]he percentage of all antibiotic prescriptions given to treat conditions they’re useless against was even higher in December 2021 than it was before the pandemic began.” (It didn’t help that a bunch of those scripts were supposed to treat Covid-19.) Some groups of people were more likely to receive inappropriate antibiotics. At the end of 2021, 30% of antibiotics for older adults with Medicare Advantage coverage were inappropriate, compared with 26% of antibiotics for adults with private health insurance and 17% of antibiotics for children with private insurance. * “from more than 37.5 million children and adults” Here’s a twist: Putting Neosporin (well, neomycin) in your nose might get your body to fight off respiratory viruses. Not that the ointment itself does the job — rather, Yale researchers found, it “triggered a swift immune response from genes in the human nose that serve as a first line of defense against invading viruses.” [T]he researchers found that mice treated intranasally with neomycin showed a robust [interferon-stimulated genes] line of defense against both SARS-CoV- 2 and a highly virulent strain of influenza A virus. Oh, and they tested it on humans, too, and found the same response. The question is how long the response lasts. Would you need to rub it in your nose every day, or just once? Stay tuned. Maybe if you believe social media (or the quality journalism in the NY Post or Daily Mail). They also help with knee osteoarthritis. It’s not surprising, really, but the question is whether that will ever be an approved use. During the pandemic, obviously states with more rules for nursing homes had fewer cases and deaths (thanks to slowing the virus’s spread). Wrong! A team led by folks at Columbia University compared the number of Covid-19 policies in a state to the number of cases and deaths in nursing homes and home healthcare agencies. Turns out that having more anti-Covid policies in place “wasn’t consistently tied to lower community- or [nursing home]-level disease burden.” “For example, on May 24, 2020, Montana, Hawaii, and Alaska had no Covid-19 deaths or policies, in contrast with North Carolina’s moderate burden and several policies.” […] “By January 12, 2021, New York had a severe Covid-19 burden and the greatest number of policies, while Pennsylvania, Montana, and Florida had a similar Covid-19 burden but fewer policies.” So why was it such a crapshoot? Implementation and compliance. Just having policies on paper — and not actually enforcing them (or facilities being unable to implement them) — means that the data won’t line up. How do you make a shortage of growth hormone for kids even worse? By throwing insurance companies and prior authorization into the mix. [P]atients and doctors are chasing whatever size injection pen and whatever brand is available. That triggers insurance companies to ask for a new prescription and new prior authorization every time patients need to switch gears and ask for a different pen size because their normal one is out of stock. So is H5N1 bird flu something we really should worry about, or just another case of ‘much ado about nothing’? It’s looking like a bit of both: Avian flu viruses tend to be picky about their hosts, typically sticking to one kind of wild bird. But this one has rapidly infiltrated an astonishingly wide array of birds and animals, from squirrels and skunks to bottlenose dolphins, polar bears and, most recently, dairy cows. In fact, viral particles are showing up in grocery milk. But there’s no need to be concerned, citizen. The good thing is we’ve got plenty of warning in case it does become more virulent, plus there’s already a vaccine.Why to worry (and not) about H5N1, plus nasal Neosporin, making the HGH shortage worse, and more
Not getting the message
Why to put Neosporin in your nose
Ozempic quickies
Do GLP-1 drugs change your personality?
But seriously, folks
Rules are apparently made to be ignored
HGH trouble
The Long Read: Bird Flu edition
April 23, 2024 ✒ Andrew Kantor
The folks at the University of Michigan’s Rogel Cancer Center have been busy studying, well, pee. First, a group of researchers found a way to use a urine sample to not only detect prostate cancer, but to differentiate the two major kinds — the slow-moving type that’s usually ‘keep an eye on’, and the dangerous aggressive type that needs immediate attention. Second, a different group “have created a urine-based test that detects pieces of DNA fragments released by head and neck tumors.” That’s important because there isn’t any kind of test available at all, other than a biopsy, for those cancers. Giving dementia patients anti-psychotic meds might be a very bad idea, according to a new, big British study: It used data from 174,000 patients with dementia, more than 35,000 of whom were prescribed antipsychotics for the first time. To cut to the chase: Antipsychotic use compared with non-use in adults with dementia was associated with increased risks of stroke, venous thromboembolism, myocardial infarction, heart failure, fracture, pneumonia, and acute kidney injury, but not ventricular arrhythmia. (Emphasis ours.) The risks of drugs like haloperidol, quetiapine, and risperidone weren’t a secret, but this is one of the larger studies to suss out the details, and it “found a considerably wider range of harms associated with antipsychotic use in people with dementia, and the risks of harm were highest soon after initiation.” Their recommendation is no surprise: The risks are serious, so “Any potential benefits of antipsychotic treatment therefore need to be weighed against the risk of serious harm across multiple outcomes.” Mmm, nothing like a glass of cabbage juice to treat what ails ya. Well, if what ails ya is inflammatory bowel disease and you’re a mouse. We all know by now how important gut bacteria are, and University of Missouri veterinary researchers found that red cabbage juice helped some good bacteria flourish in mouse guts. “Good” because they happen to produce some short-chain fatty acids that can reduce inflammation associated with IBD. Specifically… “These changes in the gut microbiota are associated with improved gut barrier function, enhanced colon repair and anti-oxidative effects, ultimately mitigating intestinal damage and colonic inflammation.” Drink up! We won’t tell if you won’t: Changing a patient’s diet might treat the symptoms of irritable bowel syndrome better than drugs do. Swedish researchers tested two diets against standard IBS meds. The first diet included smaller and more-frequent meals and fewer foods with lactose, as well as cutting back on legumes, onions, and grains “which ferment in the colon and can cause pain in IBS.” The second group went with low carbs and higher protein and fat. The third group took whichever drugs were recommended based on their individual symptoms. In the end, 76% of the first diet group saw reduce symptoms, 71% of the second diet group did, while only 58% of the medication group got relief. (For what it’s worth, all the subjects “reported significantly better quality of life, [fewer] physical symptoms and [fewer] symptoms of anxiety and depression.”) Choose a female GP, especially if you’re a woman. A new study out of Japan — based on US Medicare data — found that “Being treated by a female physician can reduce the risk of death and hospital readmission.” Based on data of almost 800,000 male and female patients over three years, it found a “large and clinically meaningful” difference for women seeing female docs, and a small difference for male patients. To be fair, their definition of “large and clinically meaningful” doesn’t seem large: There was an 8.15% mortality rate when seeing a female physician, vs. 8.38% when the physician was a man. Still, if you’re rolling the dice you want the best odds you can get. (And you can bet that little detail won’t appear in a lot of news stories.) Oh, and “Both women and men had a lower adjusted readmission rate when treated by a female physician.” Hospitals, it seems, are still using older, generic antibiotics even when patients have resistant infections, and even when there are newer, better drugs available. A study from the NIH (with Emory and George Washington universities) found that not only were hospitals behind the times, “nearly 80% of the time these older agents are already known to be highly toxic or sub-optimally effective.” Why? A few reasons. In some cases, physicians preferred to use the newer drugs only on “difficult-to-treat bloodstream infections and those with a high comorbidity burden.” Some hospitals — such as smaller facilities and those in rural areas — tended not to have those drugs available, likely because of the low prevalence of resistant infections. And then there’s the cost, as hospital reimbursement can be lower for newer, higher-priced medication. (“Sorry, we’re not giving you the best drugs because that’s less profitable for us”?) * “Meropenem–vaborbactam, eravacycline, imipenem–cilastatin–relebactam, and cefiderocol,” in case you’re interested Semaglutide helps something like 86% of patients lose weight. But what about that other 14%? Failing to lose weight could be due to a number of factors, so Healthline offers “5 reasons you may not lose weight on drugs like Ozempic or Wegovy.” (Really it’s just four reasons, because one is ‘Not taking the medication’ — that doesn’t count.) Most people know that a downside to GLP-1 agonists for weight loss is that once you stop taking them, you’ll probably gain back the weight you lost. But why? Can’t you lose the weight, then change your lifestyle to keep it off? An Aussie GP explains why, while that might be possible, it’s not simply a matter of willpower.Why Ozempic can fail, P is for a pair of cancer tests, when to drink cabbage juice, and more
Urine at the U of M
Antipsychotics and dementia don’t mix
Juice of the cabbage (and IBD)

Diet vs drugs against IBS
Want to live forever?
With meds, what’s old is sometimes just … old
Ozempic answers
Why doesn’t it work for everyone?
What happens when you stop?
April 20, 2024 ✒ Andrew Kantor
The latest poll about healthcare trust has some bad news for pharmacists: Trust in them (that is, you) dropped 3 percent from 2023 to 2024. That was only half the drop that trust in “friends and family” saw; maybe they got tired of being told, “No, dear, watermelon won’t cure your ingrown toenail no matter what you saw on TikTok.” Trust also dropped in pharma companies, government leaders, and journalists — all likely because people think they can find better information on their own. “The rise of empowerment is potentially something great,” said the CEO of Edelman Trust, which conducted the survey. “But without it being balanced with some form of trust in institutions, trust in expertise — if it’s all self-reliance, it’s like giving a kid the keys to a car and saying, ‘Go drive!’” The problem, of course, is that “empowerment” for many people means “believing whatever nonsense is being spouted on social media,” leading to people thinking mRNA vaccines contain nanobots, or that drinking bleach can treat Covid. Hey, pharmacists and pharmacy techs — want to learn about Abbott’s new FreeStyle Libre 3 continuous glucose monitor? How about if Abbott threw in a free dinner to go along with it? If you’re in the Columbus area this coming Tuesday, April 23, register for the aptly named “An Overview of the FreeStyle Libre 3 system.” The program is at Mabella Italian Steakhouse* at 6:30 p.m. and includes dinner while you listen to Bantwal Baliga, the director at East Alabama Endocrinology. Like we said, the program and food are free — but you do have to register. Click here to do that, then enter meeting ID 11165. * 6835 Midland Commons Blvd in Columbus (map) The good news for Eli Lilly is that Zepbound (tirzepatide) was shown in phase-3 trials to work against obstructive sleep apnea. It makes sense, of course. As GLP-1 drugs help treat obesity, they also help with the side effects, from heart issues to sleep apnea. The important part is getting FDA approval to treat those on-label, which would mean more insurance coverage for the drugs. …is that supply problems continue for Zepbound and other GLP-1 agonists. The drug isn’t expected to be out of shortage until June. The reason is simple: “insatiable demand.” Diabetes, obesity, heart issues, sleep apnea … what else might Mounjaro, Ozempic, and Zepbound be able to treat? How about fatty liver disease, kidney disease, brain disorders, Parkinson’s, Alzheimers, depression, bipolar disorder, anxiety … heck, just throw a dart at an ICD-10 chart. Forbes has the full rundown of what scientists are looking at. After pledging to lower the costs of its Flovent asthma med, GSK went and pulled it from the market, leaving generic fluticasone in its place — without that $35/month guarantee. Oh, well. Worse, the generic version still isn’t covered by many insurers, so American kids can’t get their daily-use inhalers unless their parents shell out the big bucks — or convince the insurers to pay for it. You would think insurance companies would be happy to cover cheaper generics, but you’re forgetting one thing: kickbacks. Insurers and PBMs don’t get kickbacks from drug makers on generic products, only on branded ones, so why bother covering the generics? That wouldn’t be good for shareholders, would it? GSK says its new, first-in-class gonorrhea treatment, gepotidacin, has passed its phase-3 trials with a 90+ percent success rate. That’s good news, what with STDs running rampant these days. Drug shortages here are a problem, but they’re worse overseas — specifically, in Britain, where they’re dealing with not only the general Europe-wide issues, but the continued fallout from Brexit. “Drug shortages in the UK more than doubled between 2020 and 2023 with Brexit likely to ‘significantly weaken’ the country’s ability to tackle supply chain snags.” Women have been dealing with menopause for a couple of hundred thousand years, and yet there’s still a bit of a stigma talking about it, the effects it can have on a woman’s body, and ways to help alleviate some of those negative issues. Worse, as this article in the Atlantic explains, many gynecologists will try to solve everything with estrogen (or, if they’re British, oestrogen). Since the 1960s it’s been the go-to magic bullet for women in and after menopause. Reality, though, is more complex — and we’ve learned a lot since the ’60s. Still, though, the lack of a “frank approach to sexuality” for both people born female and those who have transitioned there has kept many from realizing the benefits of other hormones. (Ironically, trans women often get better care when it comes to hormones.) The point of all this, and of the Atlantic article, is that it’s important for women to think beyond estrogen.Kids can’t get asthma meds, losing trust in pharmacists, looking beyond estrogen post-menopause, and more
Trust issues
CGM info and a free dinner, on Abbott
Ups and downs for Lilly
But the bad news….
On the subject of GLP-1 agonists
Please, sir, can we have our asthma meds?
Short takes
New antibiotic for gonorrhea
Elsewhere: Could Be Worse edition
The Long Read: menopause, estrogen, and women’s unused options
April 18, 2024 ✒ Andrew Kantor
We’ve covered the dangers of melatonin gummies a couple of times, whether it’s parents giving too much to kids, or kids popping them thinking they’re candy. Now, finally, someone has come up with a crazy idea to hopefully reduce some poisonings: labelling the bottles. The Council for Responsible Nutrition — the trade group for supplement manufacturers — has announced that it’s adopted new guidelines such as … All the guidelines are voluntary, and the CRN suggests they be implemented within a year and a half to 2 years. One good thing about US drug makers being so profitable is that those profits trickle down — after all, they’re paying a ton in taxes. Oh, wait. Corporations are supposed to pay a nominal tax rate of 21%. But in recent years, the biggest pharmaceutical companies had an average effective tax rate of less than 12%, according to an analysis by the Senate Finance Committee. The game, it seems, is to create a subsidiary outside US jurisdiction, sell that subsidiary your intellectual property rights, then “pretend like the profit is accrued to these offshore subsidiaries, even though the sales are back to the United States.” And thus, the “financial records for the top five drug companies in the U.S. showed that in 2023, all but Eli Lilly reported losing money in the US.” (Emphasis ours.) That’s right: When it comes to paying their share, the big pharmaceutical companies claim they’re losing money. Deadly bacteria — just like vampires, mosquitoes, and (according to Facebook) some politicians — are apparently drawn to the scent of blood. “We learned some of the bacteria that most commonly cause bloodstream infections actually sense a chemical in human blood and swim toward it.” Washington State University researchers say it’s one reason some conditions, like inflammatory bowel disease, can be deadly: Bacteria head straight for any internal bleeding. Having found the mechanism, they now hope to find a way to block it. This one comes out of the University of California-Riverside and it would be “universal” for a given disease (e.g., flu, Covid) “because it targets a part of the viral genome that is common to all strains of a virus.” So in the case of the flu, no more guessing the next year’s strain, and in the case of Covid-19, no more playing Whac-A-Mole™ with variants. The new strategy does away with Ye Olde strategy of getting the immune system to mount a response. Instead, it relies on the production of “interfering RNA” (RNAi) molecules that the body produces to attack a virus. Normally, a virus can block enough RNAi to thrive, but the UCR-developed vaccine counters this, leaving the virus vulnerable to RNAi attacks. “[The virus] can replicate to some level, but then loses the battle to the host RNAi response.” [T]he researchers say there is little chance of a virus mutating to avoid this vaccination strategy. “Viruses may mutate in regions not targeted by traditional vaccines. However, we are targeting their whole genome with thousands of small RNAs. They cannot escape this.” Pharmacists at two Rhode Island CVS locations … … are seeking to join the Pharmacy Guild, a U.S. trade union exclusively specializing in representing and unionizing pharmacy professionals, to fight for higher staffing levels, which they argue will lead to optimal patient safety and care outcomes. To fight postpartum depression, a quick dose of esketamine might be the ticket. Chinese researchers found that, at least for mothers with prenatal depression… …a single low dose of esketamine after childbirth decreases major depressive episodes at 42 days post partum by about three quarters. To get a jump on the next pandemic, the US will be partnering with 50 nations around the globe (or across the globe for you flat-Earthers). The idea is that we’ll help them “prevent, detect, and effectively respond to biological threats.” That way if something appears first in, say, East Freedonia, the Freedonians can slow its progress enough for America to be better prepared. The WHO has been trying to get an international pandemic plan in place, but that hasn’t happened. So here we are. (This isn’t just a “Hey, we’re gonna do this” announcement. It’s actually a huge program that’s well underway. Check out the State Department details. The Chinese government, it seems, is giving tax rebates to “companies that manufacture fentanyl analogues, precursors and other synthetic narcotics, so long as they sell them outside of China,” according to a report from the bipartisan House of Representatives’ select committee on China. For its part, Chinese officials pinkie-promised that they’re cooperating with US drug authorities to try to limit fentanyl production. They also said that the problem is US demand, not Chinese supply. Quoth: “It is very clear that there is no fentanyl problem in China, and the fentanyl crisis in the United States is not caused by the Chinese side, and blindly blaming China cannot solve the U.S.’s own problem.”Pharma companies losing money? Plus blood-hunting germs, warnings on melatonin, and more
The least they could do
The word is chutzpah

Out for blood
The next universal vaccine candidate
Short Takes
Elsewhere: CVS pharmacies look to unionize
Ketamine after birth
Preparing for the next one
With friends like these
April 16, 2024 ✒ Andrew Kantor
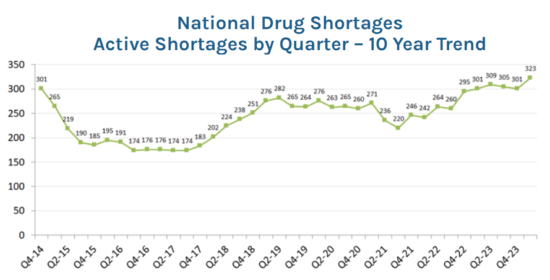
If a patient has a bacterial infection in the lower lungs, antibiotics would seem to be a good choice to treat it. Wrong. Researchers from Georgetown, the University of Wisconsin, and UGA found that that giving antibiotics to treat a cough — even when it’s caused by a bacterial infection — usually doesn’t work. The antibiotics prescribed in this study for lower-tract infections were all appropriate, commonly used antibiotics to treat bacterial infections. But the researchers’ analysis showed that of the 29% of people given an antibiotic during their initial medical visit, there was no effect on the duration or overall severity of cough compared to those who didn’t receive an antibiotic. Combined with simply not knowing whether a cough is bacterial or viral (and of course the whole overuse-of-antibiotics concern) it’s probably best to use “Basic symptom-relieving medications plus time.” Drugs in shortage have hit their highest level since 2001, according to data from the American Society of Health-System Pharmacists — that’s as far back as it tracked those numbers. Most medicines in active shortage at the end of March were central nervous system drugs, with 66 on the list, followed by antimicrobials at 43. Rounding out the top five are hormonal agents (34), chemotherapy (32) and fluids and electrolytes (25). Until the president is willing to press the big red “Lower Drug Prices” button on his desk*, there’s a lot of blame and speculation going around — it’s almost as if there are several issues at work. The DEA’s opioid reaction of tightening restrictions are a part. Wholesalers are a part. Drug companies are a part. You get the picture. Here’s an interesting tidbit: “[A] vast majority (60%) of manufacturers told the University of Utah Drug Information Service that they do not know or refused to provide a potential reason for the shortages.” The 40ish percent who did reply assigned blame equally to supply/demand, manufacturing issues, or “business decision.” * It’s right next to the “Lower Gas Prices” button. One of the issues with drug shortages is the competing priorities: Independence from Chinese manufacturers and an uninterrupted supply of critical meds. For example, one of the Chinese companies that Congress is investigating for its ties to the Chinese government also happens to make “blockbuster drugs for the American market that have been hailed as advances in the treatment of cancers, obesity and debilitating illnesses like cystic fibrosis.” No simple answers, huh? A new study out of Iran found that a combination of probiotics and vitamin D “significantly improves cognitive function in schizophrenic patients.” It was a small study (69 patients) based on the idea that both “good” gut bacteria and vitamin D can regulate the kind of inflammation that might be associated with schizophrenia. We say “might” because the causes of schizophrenia still aren’t clear. (“It has been suggested that anti-inflammatory strategies can be effective in the treatment of schizophrenia.”) They also suggested that “In the pathogenesis of schizophrenia, vitamin D deficiency is an important factor.” This is one of those studies that gets put in the ever-growing pile of “Data that might lead to a path that leads to a treatment.” We might be on the cusp of a ia vaccine. It’s still in the early-trial stage, but UK infectious-disease researchers — with help from some of those shifty Danes — have developed “CTH522,” which uses and outer membrane molecule of the Chlamydia trachomatis bacteria to create an immune response. Chlamydia, as you probably know, is the most common STD in the country and is easily treatable … if it’s found. It usually doesn’t present symptoms in women, but it can cause a lot of issues including vision loss and the inability to get pregnant. And with STD rates skyrocketing in these parts, a vaccine would be a Very Big Deal. Still, the vaccine candidate is very much in the early stages, but the fact that it exists at all is good news. In addition to all its other issues, the flu causes collateral damage to lung tissue — potentially life-threatening damage. Now, though, scientists at four major research institutions* have developed a drug that not only protects against that lung damage, but also “seemed to improve the adaptive response against the virus.” Well, in mice at least. Still, the drug “UH15-38,” removes one of the deadliest aspects of the flu for those mice: the inflammation that permanently damages the lungs. Some inflammation is good, as it means the immune system is in gear. But too much, obviously, can be a big problem. Here comes the science: The collaborating scientists achieved a Goldilocks amount of inflammation using clever chemistry. Their new drug inhibited one part of a major inflammation protein in immune cells: Receptor-Interacting Protein Kinase 3 (RIPK3). RIPK3 controls two cell death pathways in response to infection: apoptosis and necroptosis. Necroptosis is highly inflammatory, but apoptosis is not. Both pathways are used in the antiviral response. UH15-38 was designed to prevent RIPK3 from starting necroptosis while maintaining its pro-apoptotic properties. Even better, unlike current flu treatments (i.e., Tamiflu), UH15-38 works even if taken 5 days after initial infection. * Fox Chase Cancer Center, St. Jude Children’s Research Hospital, Tufts University School of Medicine, and the University of Houston If your garage is filled with a variety of chemicals — old paint, car fluids, that rusted can of something of Uncle Sonny’s — you might be increasing your risk of amyotrophic lateral sclerosis, aka ALS*. University of Michigan researchers knew that exposure to heavy-duty toxins at work was dangerous, but when they looked at home storage (i.e., in the garage), they found that even casual woodworkers and gardeners were at risk. Through statistical analysis, they found that the storage of chemicals — including gasoline and gasoline powered equipment, lawn care products, pesticides, paint and woodworking supplies — were significantly associated with ALS risk. The good news is that this only applies to attached garages. Detached ones are only risk if you spend too much time there. * Once called “Lou Gehrig’s Disease” until we learned that it isn’t what he actually had.Drug-shortage record, potential chlamydia vaccine, death in the garage, and more
When antibiotics fail (even though you’d think they would work)
Drug shortages set new record
In a related story….
Supplements for schizophrenia?
Let’s applaud these scientists
Stopping flu’s deadly side
Bad chemical romance
April 13, 2024 ✒ Andrew Kantor
No one likes a bitter drug — coffee being the exception — and usually the solution is “Buck up, little soldier.” But there might be a solution, according to the folks at the Monell Chemical Senses Center (“Advancing discovery in taste and smell”): rosiglitazone, the diabetes drug. Apparently it can be added to other medications to make them taste better. It’s not perfect, but they see it as a good first step towards building a better bitter blocker. For now, though, “Rosiglitazone is valuable as a bitter blocker because it is potentially effective in most people and is part of a class of drugs already approved worldwide for treating diabetes.” Eli Lilly and Novo Nordisk have been fighting tooth and nail to prevent pharmacists from creating compounded versions of their GLP-1 drugs while those drugs are in shortage. Lilly just lost again in Florida where a judge tossed the company’s suit saying that it can’t “use state law as a back door to privately enforce” federal law — specifically the Food, Drug, and Cosmetic Act. The FDA is pretty clear: If a drug is in shortage, compounding it is AOK. (We’ll point out that the argument “XYZ Pharmacy is claiming to sell Ozempic™” is a legit trademark issue, but that’s different than “XYZ can’t sell compounded semaglutide.”) Just because you’ve hit 65, ladies, doesn’t mean you have to give up on hormone therapy. That’s according to the North American Menopause Society* — a new paper it published says, essentially, that fears of cancer and heart disease are unfounded … sort of. Rather, the risk is nuanced: A new large-scale study based on the records of 10 million senior Medicare women from 2007 to 2020, however, suggests that the implications of HT [hormone therapy] use beyond age 65 years vary by type, route, and dose. In other words, ‘there is no general rule for stopping hormone therapy in a woman based on age alone.’ * It now identifies simply as “The Menopause Society” Georgia got its third measles case this year according to the Department of Public Health. And no, this person wasn’t vaccinated. (He or she came here with an international group of students and is now in hospital recovering.) Three is a nice low number, but given how contagious measles is, fingers crossed that it stays low thanks to most people being vaccinated. On that subject … With 113 cases in the US so far this year, the country is poised to lose the measles-elimination status that it achieved almost 20 years ago. What does that mean? Essentially that measles cases have reached the tipping point where the disease is spreading faster than it can be contained and outbreaks continue. (“[T]here won’t be any economic, political, or practical penalties.”) While anti-vaxxers might celebrate, keep in mind that 68% of kids who contracted measles in the last couple of years required hospitalization, as well as 56% of people overall. The effects of marijuana continue to come fast and furious now that researchers can actually research it. The latest is on the plus side: Non-medical cannabis use is linked to “a lower likelihood of experiencing subjective cognitive decline.” Subjective cognitive decline is all about how participants answered the question, “During the past 12 months, have you experienced confusion or memory loss that is happening more often or is getting worse?” Individuals who used cannabis for non-medical reasons reported significantly reduced odds of experiencing subjective cognitive decline compared to those who did not use cannabis. This suggests that non-medical cannabis use, as opposed to medical or mixed-use, might have a protective association against the self-perception of cognitive decline. What was interesting to the SUNY Upstate Medical University researchers was that why people used cannabis (i.e., recreationally vs. medically) was more important than how much or what type they used. Regardless, if it turns out to be true, Shaggy and Scooby will probably be doing pretty well in their old age. This year New York implemented a new pricing-transparency law that showed just how much money PBMs got from transactions with independent pharmacies. And when they saw how much money they were losing, “Nearly all independent pharmacies surveyed across New York have stopped selling certain name-brand medications.” [P]roviders are more aware that they can lose more than $200 each time they dispense certain prescriptions. […] The most common medications they’ve stopped selling to avoid such losses include weight loss drugs Ozempic and Wegovy, Merck’s diabetes medication Januvia, and Bristol Myers Squibb’s blood thinner Eliquis. Respondents also said they’ve ceased selling Symbicort, which treats asthma, and Biktarvy, an antiretroviral medication to treat HIV and AIDS. As a spokesman for the New York City Pharmacists Society explained, “It is not sustainable economically for them to carry these drugs.” Yes, owning a cat can increase your risk of schizophrenia. A new Aussie meta analysis of 17 studies found that “cat exposure is associated with an increased risk of broadly defined schizophrenia-related disorders” but not, however, for “psychotic-like experiences.” The big caveat is that almost all of those studies show correlation rather than causation, so it might be that whatever causes someone to want a cat also causes them to develop schizophrenia*. (Above link goes to the paper. For the news story click here.) * Yes, there are jokes to be made here, but they would be in bad taste so we’ll let you make them behind closed doors. A couple of cats in Kansas caught a rare fungal infection called sporotrichosis. Normally that’s not news, but the Kansas Department of Health and Environment (and later the CDC) got involved when one of the cats scratched a vet tech and gave the infection to her. They didn’t diagnose the fungal infection quickly enough, so results could have been better. The vet tech was put on an antifungal for eight months, and her infection cleared. The first cat also got an antifungal, but she eventually got sicker, and her owners had her euthanized. The second cat was treated much more quickly and recovered. When pot is good for your brain, plus NY’s painful PBM fallout, Lilly’s latest loss, and more
Bitter battle won?
Lilly loses another case
Hormones after 65? You bet
Short takes
Georgia gets another measles case
19 years down the drain?
Marijuana vs dementia
Elsewhere: “I shouldn’t have looked”
Cat news
One flew over the catbox
Fungus among them (and us)
April 11, 2024 ✒ Andrew Kantor
Oral meds for treating a urinary tract infection aren’t anything new, but what about a vaccine? And what about one that’s a mouth spray? That’s just what British clinicians say they have in a drug called MV140. It’s given twice a day for three months — don’t worry, it’s pineapple-flavored — after which “54 percent of study participants remained UTI-free for nine years after the vaccine, with no notable side effects reported.” They had already shown it worked in the short term, and now they have the long-term safety data. Next they want to expand the test group before talking about bringing it to market. Why yes, they do call it a “game-changer.” Apparently you can treat abnormal heart rhythm at home. All that’s needed is etripamil, a nasal spray calcium-channel blocker, according to researchers at Weill Cornell Medicine. Paroxysmal supraventricular tachycardia (PSVT) isn’t usually deadly, but with shortness of breath, chest pain, dizziness, or fainting involved, it can send people to the ER and even end with short-term hospitalization. But with etripamil on hand it’s like having an asthma inhaler — patients “experienced symptom relief on average in 17 minutes.” This was the second, larger trial of the drug (more than 1,100 patients), designed to show that “etripamil is safe and effective under more real-world circumstances.” Which it did. A new drug called zilebesiran, — an investigational drug, we should point out — does well by people who can’t keep their blood pressure under control. A single injection “reduced systolic blood pressure by between 4 to 12 mmHg on average” for at least 3 months and usually twice that. The basic science: Zilebesiran works by reducing the body’s production of angiotensinogen, a hormone primarily made in the liver that helps to regulate blood pressure by constricting blood vessels. Reducing blood-vessel constriction allows blood pressure to fall. It can be used alone, but it works even better in combo with other anti-hypertensives. Big ol’ caveat: Although the study was done out of Brigham and Women’s Hospital in Boston, it was funded by Alnylam Pharmaceuticals, the manufacturer of zilebesiran. Take from that what you will. The Dawgs moved up nine spots in the US News & World Report rankings of US pharmacy schools, now coming in at #15 out of 141. High-five! Pfizer says its Abrysvo RSV vaccine works a treat for folks under 60. It’s going to ask for approval for the vaccine at least for high-risk people in the 18-59 category. Ka-ching! Acetaminophen during pregnancy doesn’t increase the risk of having a kid with autism, ADHD, or an intellectual disability — so says a big US/Swedish study using data from 2.4 million Swedish kids, including 186,000 whose mothers used acetaminophen during pregnancy, even if they called it “paracetamol.” Imagine what went down at Nature Made HQ: Marketing director: I’m going on vacation for two weeks. Don’t do anything stupid while I’m away. Jimmy from marketing: Sure thing, boss. So, everyone, what sports seasons are starting soon? Kevin from marketing: Baseb— Susan from marketing: April is National Pickleball Month! Jimmy: Great! How can we celebrate it? Susan: Pickled-flavored vitamin gummies! Kevin (quietly): I was gonna suggest Cracker Jack-flavored. Jimmy and Susan: Shut up, Kevin. Researchers at the University of Rochester tested a crazy They tested the ventilation in 100 rooms of various sizes on a campus for special needs kids by measuring carbon dioxide levels. Surprise, surprise! Kids who spent more time in rooms with “suboptimal ventilation” were more likely to get Covid. They also found that spending time in the rooms with newer ventilation systems (MERV-13, if you’re keeping score) reduced the incidence of Covid thanks to better filtering. Meanwhile downstate at Columbia, researchers tested ceiling-mounted far-UV lights as germ killers. “Far-UV” doesn’t hurt people (it can’t damage living skin) but it’s brutal for bacteria. They mounted the devices in a room with lab mice, where cage-cleaning releases a ton of norovirus particles, then tested the air. “Based on our initial sensitivity tests, we expected to see a reduction in airborne virus of around 66%,” said the senior author. Instead, “The result—a reduction in infectious airborne viruses of 99.8%—surpassed expectations and was far greater than what could be achieved by typical air filtration and ventilation.” Now they’re testing the lights in more locations, with the goal of being able to use the devices to keep public spaces disease-free. A nasal spray for the heart, 6-month BP drug, Nature Made’s weird decision, and more
Surprise delivery 1: Oral spray for UTIs
Surprise delivery 2: Nasal spray for tachycardia
Blood pressure: One shot for 6 months
Short takes
Congrats to UGA CoP
RSV vax for everyone?
No Tylenol/autism connection
Why not to drink at work

It’s almost as if Covid is an airborne virus
theory hypothesis: Could improving air quality and circulation cut Covid infections?Safer UV kills airborne germs

April 09, 2024 ✒ Andrew Kantor
Mess with a child’s gut bacteria in the first year and you could raise the risk that he or she develops autism or ADHD. That’s what Swedish and American researchers found after looking at the health records of 16,000 Swedish children born between 1997 and 1999 — kids the Swedes have studied over the past 25 years. “We can see in the study that there are clear differences in the intestinal flora already during the first year of life between those who develop autism or ADHD and those who don’t.” What’s going on? They think something is affecting those bacteria — e.g., antibiotic treatment. For example, “Children who had repeated ear infections during their first year of life had an increased risk of being diagnosed with a developmental neurological disorder later in life.” In fact, they’ve narrowed it down to two particular bacteria that affect risk — “the presence of Citrobacter bacteria or the absence of Coprococcus bacteria increased the risk of future diagnosis.” That info might lead to a concurrent treatment (some kind of probiotic?) to go with antibiotics. As usual, though, more research is needed. What if asthma wasn’t caused by inflammation, rather the inflammation was a result of the disease? That, say British cell biologists, is exactly the case. It’s the mechanical constriction of the airways that leads to an asthma “attack,” including inflammation. Current treatments focus on that inflammation, but that only alleviates symptoms. The issue may lie in the death of the airway’s epithelial cells: When the airway contracts, a process called cell extrusion kills the epithelial cells lining it. So many epithelial cells dying leads to inflammation and excess mucus — an asthma attack. Thus blocking cell extrusion might be a way to prevent attacks rather than dealing with symptoms. And guess what? There’s already a chemical that does that. “[A]n inhaler such as Albuterol opens the airways, which is critical to breathing but, dishearteningly, we found it does not prevent the damage and the symptoms that follow an attack. Fortunately, we found that we can use an inexpensive compound, gadolinium, which is frequently used for MRI imaging, to stop the airway damage in mice models as well as the ensuing inflammation and mucus secretion.” Don’t forget: Early-bird registration for the Georgia Pharmacy Convention ends this Thursday, April 11. Save $50 by registering by then! People who get coronary stents often continue taking aspirin after the procedure. They shouldn’t. A new study out of Mount Sinai found that the standard-of-care guidelines are probably wrong. The best thing patients can do (that we know of) is to use ticagrelor alone. “Our study has demonstrated that withdrawing aspirin in patients with recent ACS [acute coronary artery syndromes] one month after PCI [percutaneous coronary intervention] is beneficial by reducing major and minor bleeding through one year by more than 50 percent. Moreover, there was no increase in adverse ischemic events, meaning continuing aspirin was causing harm without providing any benefit.” What do you someone who tests their partner for STIs by sending a picture of his nether regions to an app? A patient. Yep, there’s an app called Calmara.ai claiming to detect sexually transmitted infections from a photo of a gentleman’s privates. In seconds, the site scans the image and returns one of two messages: “Clear! No visible signs of STIs spotted for now” or “Hold!!! We spotted something sus.” Pro tip: It doesn’t work — “Doctors say it’s a disaster”. What are Many users [on TikTok] also snack on sticks of butter as a weight loss tactic, with some using butter as a meal replacement. Add “skin issues” to the list of side effects of taking semaglutide. Specifically, a study out of Brown “found a higher incidence of ‘altered skin sensations’” among patients taking it, including dyses-, hyperes-, or paresthesia (i.e., various unpleasant or abnormal touch sensations) as well as alopecia or other “adverse dermatologic events.” Scripps Research chemical biologists have developed a vaccine against xylazine, the latest ultra-potent chemical that’s being added to street drugs (and adding to the overdose crisis). It works by training the immune system to attack the fentanyl so it doesn’t add its effect to whatever it’s mixed with. That’s important because naloxone doesn’t work against xylazine, so it’s critical to take it out of the equation. Granted this is still just proof-of-concept, but assuming the technique proves out, it could also be used to create a vaccine against fentanyl — another drug that’s naloxone-proof. Wondering how your pay stacks up against your peers in other states? The good folks at Becker’s have you covered. (Spoiler: There isn’t that much difference state to state, except maybe between the highest paying (California) and the lowest paying (Rhode Island). )A different take on asthma, how antibiotics can lead to autism, skin “issues” from semaglutide, and more
Autism from antibiotics?
Fighting asthma’s cause
Two more days!
Heart surgery? Skip the aspirin
From the Stupidity Files
Say “Cheese”
“Stupid don’t get tired.” —Alonzo Bodden
infomercials influencers peddling for health now? (spins Wheel of Idiocy) Butter. Eating sticks of butter. Why? “Proponents claim it aids weight loss by contributing to feelings of fullness and has other wellbeing benefits like improved mood and energy.”More semaglutide effects
Xylazine vaccine
Short take: Pharmacist pay by state